What is my TMJ?
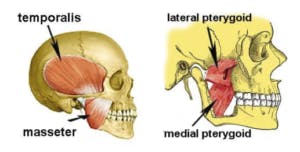
Pain with chewing can be caused by dysfunction of the temporomandibular joint (TMJ). The TMJ is formed by the mandible (highlighted in blue in the picture below) and the mandibular fossa. The mandibular fossa is a depression in the temporal bone of the skull in which the jaw bone inserts (circled in red below). If there is a dysfunction of this joint, it can lead to a plethora of symptoms including ringing or fullness in the ears, headaches, neck pain, and pain with chewing.

Pain from the joint
If there is dysfunction inside the TMJ itself, this can cause pain with chewing. When you open your mouth, the portion of your jaw that inserts into your skull must roll and glide forward. There is a disc inside the joint to lubricate this motion. Sometimes the jaw will slip forward too much in the joint when you open your mouth and slide right off the disc. This causes a popping or clunking sound and is often painful.

Pain from the muscles
The muscles of mastication (the muscles you use to chew) can also cause pain when chewing or eating. There are four muscles of mastication: the temporalis, masseter, lateral pterygoid, and medial pterygoid. All these muscles help to either open or close your mouth. These muscles can become painful with TMJ dysfunction or if they are overused such as when grinding your teeth at night. If these muscles are overused they can cause joint restrictions and headaches.
How can physical therapy help?
Physical therapy can help TMJ pain by addressing both the muscular and internal joint components of this problem through joint mobilizations and soft tissue work.