Arthritis is a condition that affects the joints, causing pain, stiffness, and inflammation. Many people with arthritis find that their symptoms can worsen as the autumn and winter seasons approach due to the cold and damp weather. Here's some information about arthritis during this time of year and what you can do to feel better:
How Autumn and Winter Affect Arthritis:
- Cold Temperature: The drop in temperature can lead to increased joint stiffness and pain for individuals with arthritis. Cold weather can cause the muscles, tendons, and ligaments around the joints to tighten, making movement more difficult and painful.
-
Dampness: Increased humidity and dampness in the air can also exacerbate arthritis symptoms. The changes in atmospheric pressure can affect the synovial fluid in the joints, leading to discomfort.
- Reduced Physical Activity: As the weather gets colder and days become shorter, people often engage in less physical activity. This reduced movement can lead to muscle weakness and joint stiffness, further worsening arthritis symptoms.
Tips for Managing Arthritis in Autumn and Winter:
- Stay Warm: Dress in warm, layered clothing to maintain body temperature. Keep joints covered to minimize exposure to the cold.
-
Heat Therapy: Apply heat to affected joints using heating pads, warm baths, or hot packs. Heat can help relax muscles and reduce pain.
-
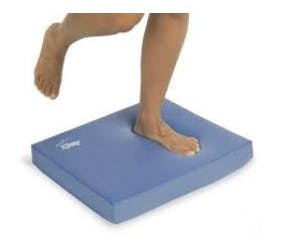
Stay Active: Engage in regular, gentle exercise to keep your joints moving. Activities like swimming, walking, or indoor exercises can help maintain joint flexibility and strength.
-
Diet and Nutrition: Maintain a healthy diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids found in fish. Some people also find relief through dietary supplements like glucosamine and chondroitin but consult a healthcare professional before using them.
-
Medications: If over-the-counter pain relievers are insufficient to manage your arthritis symptoms, consult your healthcare provider for prescription medications or injections that can help alleviate pain and inflammation.
-
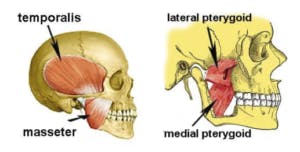
Physical Therapy: Consult with a physical therapist who can develop a personalized exercise and stretching program to manage arthritis symptoms. They can also teach you techniques for joint protection.
-
Maintain a Healthy Weight: Excess body weight puts added stress on the joints, exacerbating arthritis symptoms. If needed, work on achieving and maintaining a healthy weight through diet and exercise.
-
Manage Stress: Stress can worsen arthritis symptoms, so practice relaxation techniques like deep breathing, meditation, or yoga to help manage stress.
-
Stay Hydrated: Proper hydration can help maintain the lubrication of joints. Drink enough water throughout the day.
-
Consult a Healthcare Provider: If your arthritis symptoms worsen during the autumn and winter seasons, don't hesitate to seek advice from your healthcare provider. They can adjust your treatment plan and recommend appropriate therapies or medications.
It's important to note that the impact of weather on arthritis can vary from person to person, and what works best for one individual may not work as effectively for another. Therefore, it's essential to work closely with healthcare professionals to develop a comprehensive plan for managing arthritis and reducing its impact during the colder months.
Here are some additional ways you can learn more about arthritis and its management.
- Arthritis Foundation Website
-
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
- Consulting Healthcare Professionals: For personalized advice and treatment, it's crucial to consult with healthcare professionals, including rheumatologists and physical therapists, who can provide guidance tailored to your specific condition.