Dr. John O'Neil, DPT meets with the Athletic trainer for Loudoun Valley High School, Andrew Gordon, M.Ed., ATC to discuss how the athletes are cared for at his school
As the Athletic Trainer for Loudoun Valley High school (LVHS) for over 23 years, Andrew Gordon has diagnosed, managed, and led the rehabilitation for many students at his school who have had a concussion. A graduate of the University of Virginia for both his undergraduate and graduate studies, he has been the Athletic Trainer for LVHS since 1996, which is when he became the first full time Athletic trainer in the state of Virginia's high school systems. I had the opportunity to sit down with him and talk about the ins and outs of this ATC's view of the rehabilitative process of concussions, and how it is managed at LVHS.
What is a Concussion and how does it occur?
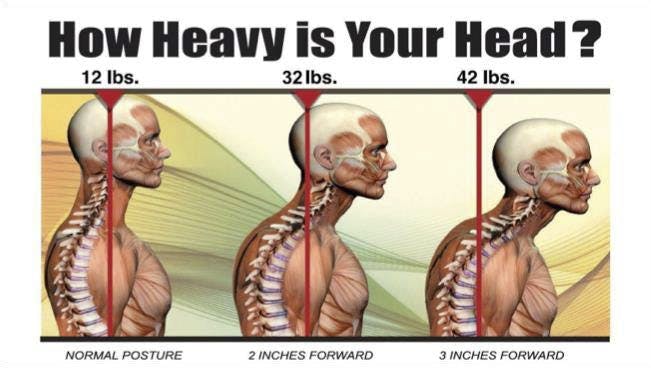
It is a complex pathophysiologic process affecting the brain, induced by traumatic biomechanical forces secondary to direct or indirect forces to the brain. This can result in a variety of physical, cognitive, emotional, or sleep-related symptoms. With a concussion, neuro-imaging is typically normal, and the duration of symptoms is highly variable - from several minutes to days, weeks, months, or longer in some cases. After the injury there is a metabolic crisis, resulting in an increase in energy demand with a decrease in blood flow to the brain. It is important that during this time of the crisis that the athlete does not get hit again as it can create compounding stress to the brain.
In the United States, there are approximately 300,000 concussions injuries each year. A large percentage of total concussions happen to the youth, with 70.5% of sports & recreation-related traumatic brain injury ER visits were among persons aged 10-19 years.
With athletes in particular, it is essential to take them through a progressive, stepwise return to play protocol to ensure safe return to play. It is just as important for the youth and the parents to understand the signs and symptoms of what a concussion is, as it is not as strait forward as one might think.
What are the signs and symptoms of a concussion?
It is important to note that the presentation of concussions can vary, and if there are any signs/ symptoms of a concussion, per Virginia state High School guidelines, the athlete will be immediately taken out of play for the remainder of the day to protect the athlete. Also, a loss of consciousness is not required for the athlete to sustain a concussion.
- Cognitive Symptoms: Fogginess, difficulty concentrating, memory deficits, cognitive fatigue
- Somatic Symptoms: Headache, dizziness, nausea, light/sound sensitivity
- Mood Disruption: Irritability, feeling sad, anxiety
- Sleep alterations: Difficulty falling asleep, fragmented sleep, too much/little sleep
When does the athlete return to play?
Concussions, and the direct or indirect contact that resulted in a concussion can affect a variety of structures in the body, and thus a variety of testing needs to occur. This includes the assessment of strength/range of motion, oculomotor screening, vestibular testing, balance, and gait testing.
Additional criterion prior to return to play include:
- Clear oculomotor exam
- Clear vestibular exam
- Symptom free with cognitive or physical exertion
- Able to handle a full day/schedule at school
- Normal neurocognitive data

Questions with Andrew Gordon, M.Ed., ATC
What is done in the pre-season at Loudoun Valley high school (LVHS) for concussions?
For the Athlete: The individual has to sign a form (along with the parents) prior to play indicating the
return to play protocol and signs/symptoms of a concussion. IMPACT test baseline testing is performed for freshman and juniors, or individuals new to sport. Individuals in low-contact sports do not need to take this test, as the incidence of concussions is very low. The highest incidence for boys is football, and for girls, soccer.
For the Parents: Andrew Gordon gives a parent meeting informing them about the concussion protocol at LVHS.
For the Coaches: Required completion of yearly concussion online course.
What happens when an athlete has a suspected concussion?
On field testing: If the individual has a potential mechanism of injury, and has any signs or symptoms, the athlete is done for the day. He then re-evaluates them the next day, and if a concussion is diagnosed by Andrew Gordon, it is a minimum 5 day recovery period to return to sport. The majority of concussions happen during games/matches of contact sports, all of which are required to have an ATC present.
In the Classroom, after injury: Andrew implements classroom accommodations as needed to not stress the healing individual, and to insure proper recovery. This can range from using sunglasses at school, no white boards, time allowed for each class, and getting the athlete out of the classroom prior to a fire drill.
Can sensors in the helmet help prevent or help identify concussions?
Short answer: No.
Long answer: This item has been extensively studied and has not been found to help identify concussions, and has resulted in many unnecessary evaluations that do not lead to better outcomes. Aside from concussions, valid sensor technologies can offer objective data that have been used to improve player safety and reduce injury risk, although this would be more for research purposes, rather that injury identification.
Message for the students?
Report your symptoms! With proper management of a concussion, you are much more likely to return to play faster than if you had pushed yourself through the symptoms. If you give Andrew Gordon 2-3 days now, you don't have to give him 2-3 weeks later. The goal is to get the athlete ready for playoffs, as he is looking more for the long term health of the athlete.
Message for the parents?
Same as the students, keep an eye on the symptoms, especially during academic tasks. Pushing the individual too much cognitively or physically can delay rehabilitation. Simple items such as looking at phone/television screens can sometimes over stress the individual, and delay rehab.
Time to Take a Stand!
Physical therapists use sound, scientifically proven principles of human anatomy, physiology, movement and psychology to help patients lead healthy, pain-free lives.
The therapist will conduct an initial evaluation followed by several progress notes to document progress over time. A comprehensive analysis establishes a 'clinical baseline' and identifies muscle imbalances, causes of pain and joint alignments. This is the foundation for short and long-term goals designed to help individuals recover completely. In fact, physical therapy can address every aspect of recovery including:
- Strength/Range of motion
- Ocular motor screening
- Vestibular testing
- Balance/gait testing
Superior Physical Therapy and Sports Rehab
- Spring Ridge
9093 Ridgefield Dr., Suite 201
Frederick, MD 21701
Phone: 301-696-5595
- Thomas Johnson
65D Thomas Johnson Drive
Frederick, MD 21702
Phone: 301-663-7898
- Purcellville Orthopedic Physical Therapy
850C East Main St.
Purcellville, VA 20132
Phone: 540-751-1970
- Frederick Indoor Sports Center (FISC)
1845 Brookfield Ct
Frederick, MD 21701
Phone: 301-663-7896